Videos
Latest News
Latest Videos

More News

Sharon Ward-Fore, MS, MT(ASCP), CIC: “If it were my institution, I would make sure that infection preventionists are educated on everything they need to know about the COVID vaccine, as well as the flu vaccine side effects.”

Rebecca Leach: “I think the biggest thing is just having support, whoever it is. If it’s a fellow infection preventionist…. It really is that emotional support of being able to talk to each other about your experiences and really process your feelings.”

Kevin Kavanagh, MD: “I would tell the Supreme Court that it’s very important that all high-risk venues are treated equally, but the remedy isn’t opening up one high-risk venue, the remedy should be closing down all high-risk venues.”

Susan E. Campbell, PhD, CIC, offers advice to infection preventionists and other healthcare professionals who’ll be working Thanksgiving on how to safely eat their holiday meal together.

Kevin Kavanagh, MD: “We can’t just bury our heads in the sand and bleed through healthcare staff and bleed through PPE, thinking that this is not going to be something that’s going to cause severe problems in these individuals, or that it’s going to magically disappear next week."

W. Frank Peacock, MD, FACEP, FACC, FESC: “When I intubate somebody, I need to know where the tube is, and I need to know now—like within 10 seconds. You can’t tell with anything else. Nothing is as fast as the stethoscope. I can get an X-ray, but I’ve got to wait for the X-ray while you hold your breath.”

Caitlin Stowe, CIC, MPH, CPHQ, VA-VC: “The cool thing about being an infection preventionists is that I call myself the jack of all trades, but the master of really none. Because you really have to know a little bit about everything.”

Linda K. Groah, MSN, RN, CNOR, NEA-BC, FAAN: “Historically, we have not always had the best relationship. There’s been some competition between infection preventionists and OR managers or directors. The operating room has been that secret area behind the double doors.”

Michael Millenson: “When you dig a little deeper, you end up though with some questions. We’re a big country, and this is an enormous crisis. Well, $180 million? You can barely buy a couple of US senators with that.”

Fibi Attia, MD, MPH, CIC: “There is a daily meeting where we talk about the possibility of getting those COVID vaccines and where are we going to store them. How are we going to distribute them? How many doses do we need? Those kinds of things are being discussed on a daily basis.”

Susan R. Bailey, MD: “Vaccine hesitancy was a huge problem before the pandemic began and has certainly not gotten better since we’ve had COVID and now are looking forward to a COVID-19 vaccine.”

Linda Spaulding: “Infection preventionists, put your tennis shoes on because over the next two months, we’re predicting to see a huge increase.... We have all the holidays coming up. You’re going to have cases from those. Hospitals have to be prepared.”

Ashish Diwanji: “The personal protective equipment made and sold in the US has to abide by the standards set up by NIOSH …. The PPE made and sold from China do adhere to the Chinese standards, but their standards are different than ours.”

Kevin Kavanagh, MD: “Infection preventionists will need to make sure that they still have access to adequate PPE, even if the vaccine comes out [and they] really need to look at the experimental group that was used for the EUA.”

Michael Bell, MD: “The challenge that infection control professionals face has grown tremendously. We’re asking these individuals to not only be experts, but also to take responsibility for such a wide range of activities ... and finding ways to help them accomplish what they’re doing across the whole population of healthcare personnel is the rationale behind Project Firstline.”

Sharon Ward-Fore, MS, MT(ASCP), CIC: “I’m hoping that healthcare facilities will find the value in their infection preventionists and understand how important a role they play as far as training on PPE and disinfectants, and in hand hygiene, being kind of a boots on the ground people on the floor to see things firsthand.”

Franklin Dexter, MD: “I would recommend to those people working in different surgical suites to recognize that within an operating room, you shouldn’t assume that stepping away from the patient would put you in reduce risk. You should think about what the airflow is in the operating room.”

Maya Gossman, RN: “Our infection preventionist has trained me in the past with the PPE use and the infection prevention measures. And so, I’m passing that on—the knowledge that she’s given me—I’m passing that on at this point to my vascular nurse trainees, my orientees.”

Monica Gandhi MD, MPH: “We will get to the end of this [COVID-19]. We will get to a combination of vaccine and natural infection, enough people getting herd immunity that this will stop. This will stop and we will get back to normal.”

Mary Jean Ricci MSN, RNBC: “In most facilities, the infection preventionist is the person doing contact tracing, is assisting the students should there be an exposure, is assisting with providing education on site or real-time education with the students should they see the students take off their PPE.”

Christopher Blank, CIC, MPH, an infection preventionist with BJC Healthcare, sits down with Infection Control Today® to discuss the benefits of making employment for healthcare workers contingent on getting the flu vaccination.
Kevin Kavanagh, MD: “Many of the infection preventionists over the last six months now have more experience than many of the policymakers up in D.C., because they’ve lived it firsthand. And they’ve seen how COVID-19 can spread. And they’re starting to develop a good idea of how to stop it.”
Sarah Smathers, MPH, CIC, FAPIC: “I think that hospital administrators are concerned about how they’re going to recruit in a field that is expecting a lot of retirees: 40% of infection professionists are expected to retire in the next five to 10 years.”

Bilal Naseer, MD: “Nurses who are kind of at a point where they cannot do bedside care, they should consider infection prevention. We need more infection preventionists.”
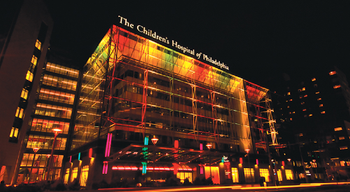
Cedric Steiner, MBA: “When we talk about infection control, and not just one room, but pieces of the facility, we’re definitely on the right track. And I think we need to start thinking about the building as like a living, breathing kind of thing.”