News








According to the CDC, roughly one in every 25 hospitalized patients has at least one healthcare-associated infection (HAI).1 HAIs create significant health risks and cost the healthcare industry billions of dollars each year.
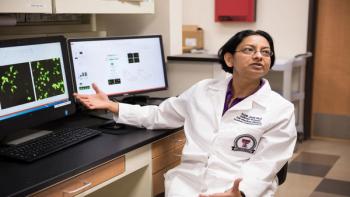
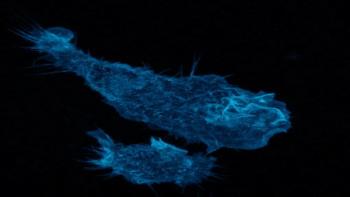
Texas Tech University Health Sciences Center El Paso researchers Anjali Joshi, PhD (pictured), and Himanshu Garg, PhD, have received a $420,000 NIAID grant to investigate the effect of previous exposure to West Nile on Zika symptoms. Courtesy of TTUHSC El Paso/Tommie Morelos West Nile virus is no stranger to the U.S.-Mexico border; thousands of people in the region have contracted the mosquito-borne virus in the past. But could this previous exposure affect how intensely Zika sickens someone now? That's what two researchers at Texas Tech University Health Sciences Center El Paso(TTUHSC El Paso) are investigating. Their findings could predict how some populations will react to Zika, a mosquito-borne virus -- and relative of West Nile -- that's slowly spreading in the states. "For those who already have been infected with West Nile, there are two possible outcomes," says Anjali Joshi, Ph.D., an infectious disease researcher at TTUHSC El Paso. "The exposure could either help inhibit Zika infection, or make it much worse."Joshi and co-investigator Himanshu Garg, PhD, were recently awarded a two-year, $420,000 grant from the National Institute of Allergy and Infectious Diseases (NIAID). The funds will help the team collect blood samples from 500 El Pasoans and test the samples for the presence of West Nile antibodies. These antibodies would indicate that the individual once had the virus, but successfully fought it off. The researchers will then use the samples to explore a phenomenon known as antibody-dependent enhancement (ADE), where the presence of certain antibodies can either fuel or fight a subsequent infection. A well-known occurrence of ADE has been observed in people with Dengue, another related mosquito-borne virus. When an individual is bitten for the first time by a mosquito carrying Dengue, their infection is usually mild. Down the road, however, subsequent bites with a different strain of Dengue -- Dengue comes in four distinct strains -- will likely lead to much more severe symptoms. "In Dengue, these preexisting antibodies enhance the uptake of the virus, making the infection more severe and the symptoms worse," Joshi explains. In other cases, the presence of certain antibodies may protect against a similar viral attack. This is the case with antibodies formed after another viral illness, tick-borne encephalitis; they protect against the Japanese encephalitis virus. Once the researchers have collected enough blood samples that are positive for West Nile antibodies, they will use them to determine if the West Nile antibodies enhance or inhibit Zika virus infection.If the results show that West Nile enhances Zika, Joshi would advise people to take extra precautions to prevent mosquito bites. Individuals may even consider getting tested for West Nile antibodies to see how careful they need to be.If the findings show West Nile inhibits Zika, however, that's particularly good news for vaccine developers, as a vaccine for West Nile could potentially protect against Zika and vice versa. Joshi hypothesizes that West Nile may have a protective effect against Zika. In another study involving mice infected with West Nile, the investigators found that serum from these mice was able to inhibit Zika virus infection in cells. Those results may not translate to humans, though, and further studies are needed before Zika becomes widespread. Garg says, "The El Paso area is endemic to West Nile Virus infection and 80 percent of people who have been infected are not even aware of the infection. The question is 'How are we going to react to Zika when it arrives? Will Zika follow the same track as West Nile?'"Source: Texas Tech University Health Sciences Center El Paso