
Sterile Processing
Latest News








For more than a millennia of medicine, the caregiver's oath has been, "Do no harm." Unfortunately for the sterile processing world, there are billions of microorganisms out there that are aiming at doing the exact opposite. The challenge is so great that most hospitals have entire departments dedicated to the mission of infection control, a practical sub-set of epidemiology concerned with preventing nosocomial (healthcare-associated) infections. Although there are countless areas of focus for these teams in a hospital setting, there are few more effective partners in winning the fight against infection than the sterile processing team.

Q: My facility does not launder our scrubs, we must take them home. I have heard from other colleagues that their facilities provide and launder their scrubs. What is the recommended dress code for SPD in the clean/sterile areas and should our scrubs be laundered by the facility?A: I can understand your confusion. Unfortunately, not all facilities comply with the standards and therefore do not provide laundered scrubs to sterile processing staff. I do not really understand the non-compliance by facilities when one considers that SPD personnel are preparing sterile product for use on patients. Therefore very effort should be made to keep bioburden levels to a minimum.








Q: My hospital is implementing a third-party reprocessing program. I am not in support of this. I cannot believe that a company can take a single-use device and make it safe again. I am all for containing costs but not at the risk of a patient safety. What do you know about this process?

Infection prevention continues to be an issue that is top of mind for GI professionals. When thinking of gastroenterology infection prevention, it traditionally has been in terms of reprocessing endoscopes and post-procedure patient phone call to assess for infections. Infection prevention for GI encompasses so much more than those two tasks - it includes correct use of personal protective equipment (PPE), personal hygiene, engineering controls of the physical environment, cleaning and disinfection of surfaces, training, continuing education, written operating procedures, and of course documentation. Earlier this year, SGNA released practice documents focused on infection prevention. The new document, Standard of Infection Prevention in the Gastroenterology Setting, brings to light an important point that is often overlooked when we discuss infection prevention: Prevention for the whole team.






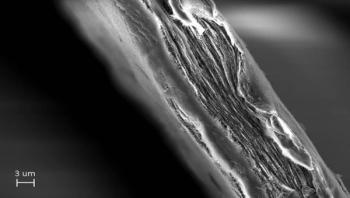
A simple paper sheet made by scientists at Uppsala University can improve the quality of life for millions of people by removing resistant viruses from water. The sheet, made of cellulose nanofibers, is called the mille-feuille filter as it has a unique layered internal architecture resembling that of the French puff pastry mille-feuille ("thousand leaves").